Postural Tachycardia Syndrome
POTS: The BasicsFind links to in depth information and resources for POTSies at on our Dysautonomia SOS website (under construction).
POTS is short for Postural Orthostatic Tachycardia Syndrome. It is referred to by some physicians and researchers as Postural Tachycardia Syndrome, or just Postural Tachycardia. It is a type of Orthostatic Intolerance, and also a type of Dysautonomia. Let’s break down what that name means:
Postural means relating to posture, or a change in position.
Orthostatic means relating to, or caused by erect posture (standing up).
Tachycardia refers to a rapid heart rate.
Syndrome means a collection of symptoms, and not a disease. Technically, a syndrome is defined as a group of signs and symptoms that occur together and characterize a particular abnormality.
So, POTS is a collection of symptoms that result from a heart rate increase when standing up. When a person with POTS stands up, the heart pumps faster to help keep the blood pressure up, and try to help the blood in their body reach their brain and other vital organs. The body of a person with POTS does not respond to gravity the same way a non-POTS person does.

The majority of POTS patients are female, of child bearing age, and under 35. There are thought to be anywhere from 500,000 to millions of people in the US with POTS and other forms of Orthostatic Intolerance. There are no solid published statistics or data at this time, these are estimates from the major research centers that treat POTS.
DIAGNOSIS:
In order to meet the most recent POTS criteria for diagnosis, a person’s heart rate must increase at least 30 beats per minute (BPM), or go above 120 BPM within 10 minutes of standing, and for kids/teens the requirement in 40 BPM. This may happen with or without a change in blood pressure, and symptoms are relieved by lying down. The recent definitions by some doctors say that if your blood pressure drops significantly, you do not have POTS. Most researchers and physicians also include that you must have symptoms for 3-6 months.
SYMPTOMS:
POTS symptoms can come and go, and change in intensity. These are some of the more common symptoms, but by no means is a complete list. POTS is complicated because many patients have underlying or other conditions causing symptoms, and it is hard to figure out which is causing each symptom, and they can change from day to day – even hour to hour.
• Lightheadedness
• Fainting or near fainting
• Visual blurring or tunnel vision
• Palpitations
• Tremulousness (shakiness) and weakness, especially of the legs
• Fatigue
• Exercise intolerance
• Hyperventilation
• Neck pain, also called “coat hangar pain”
• Shortness of breath
• Anxiety and panic feelings
• Chest pain
• Nausea and other stomach and digestions symptoms
• Acral coldness or pain (meaning in the extremities)
• Concentration difficulties (brain fog)
• Headaches and migraines
• Sweating problems, either too much or too little
• Increased heart rate while laying down
• Foot swelling and obvious blood pooling in the legs
• An increase in adrenalin levels in the blood (called norepinephrine and catecholamines)
CAUSES:
POTS is thought to be caused by many things, which is also known as being heterogeneous. You can find an in depth discussion of these, and POTS in general, here. Some of the things thought to cause POTS include:
• Low blood volume, also called Hypovolemia.
• Blood pooling in the extremities, also known as Acrocyanosis, sometimes caused by valve or muscle pump defects in the legs, neuropathy (destruction of nerves), and low blood volume. Other diseases and conditions can cause blood pooling in the arms and legs as well.
• Autonomic Neuropathy, which is when there is damage to the autonomic nerves. Autonomic nerves are the nerves that control things that happen unconsciously, like sweating. This damage can cause problems with the signals between the brain and the body, including the heart and blood vessels. It is estimated by the Mayo Clinic that up to 50% of all POTS patients have some form of Autonomic Neuropathy.
• Denervation of the legs, or a loss of nerve supply. Causes of denervation include disease, chemical toxicity, physical injury, or intentional surgical interruption of a nerve.
• Increased Angiotensin II and decreased Nitric Oxide (NO), which causes veins to not constrict properly.
• Autoimmune Diseases such as Multiple Sclerosis, Sjogren’s, Lupus, Myasthenia Gravis, Diabetes, Guillain-Barré Syndrome, Fibromyalgia, Amyloidosis, Ankylosing Spondylitis, Raynaud’s, Celiac , Chronic Fatigue and Immune Dysfunction Syndrome (CFIDS), Chronic Fatigue Syndrome - also known as Myalgic Encephalomyelitis (ME), Autoimmune Autonomic Ganglionopathy (AAG), Sarcoidosis, and general connective tissue diseases are thought to either cause or be associated with POTS.
• Post-Viral or Sudden Onset means that something sudden triggered POTS symptoms. A virus, pregnancy, a car accident, a traumatic event (such as surgery), a growth spurt, etc… brought out the underlying condition that is causing POTS.
• There are a variety of other diseases and syndromes are thought to cause POTS, including Ehler’s-Danlos Syndrome, Adrenal Diseases such as Cushing’s and Addison’s, Mast Cell Activation Syndrome (MCAS), Lyme Disease (and associated co-infections), Mitochondrial Diseases, and Paraneoplastic neurological syndromes.
• Other conditions that can cause or have been associated with POTS include: Traumatic Brain Injuries, Chiari Malformations, Gulf War Syndrome, Heavy Medal Poisoning, Parasites (such as Chagas), Liver Cirrhosis, Mycoplasma pneumonia, the Epstein-Barr Virus, the Nutcracker Syndrome, as well as reactions to drugs and medications.
This is a LONG growing and changing list, and you can find definitions, information, and links to more information on these conditions on our website. We strongly urge you to look for the underlying cause of POTS, as stated above – it is not a disease, it is a syndrome, and once you find the cause your doctor may be able to treat the symptoms of POTS more effectively.
A full cardiac work up should also be performed if you are told you have POTS to rule out any structural or electrical issues with your heart. Conditions to rule out that may be serious or life threatening, and symptoms may mimic or cause POTS include structural abnormalities such as congenital defects or “holes” in the heart, valve defects, cardiomyopathy, and cardiac atrophy (deconditioning causing the heart to get smaller), to name a few.
TESTING AND TREATMENT:
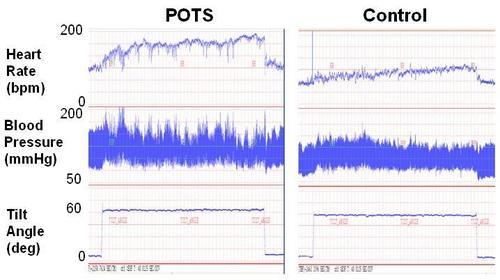
Testing depends on the symptoms of each individual patient. Find descriptions of the more common autonomic tests on our website. Additional cardiac testing or blood work may be performed as well. A thorough medical exam and history will be taken, and the most common test to diagnose POTS is a Tilt Table Test.
A Tilt Table Test, also called a Head Up Tilt Test (HUTT), measures heart rate and blood pressure when a patient goes from laying to standing. Some of these have “beat to beat” monitoring of blood pressure, which is very useful in seeing how a patients body responds to being upright.
POTS can also be diagnosed with basic orthostatic testing as well; heart rate and blood pressure are taken in the laying, sitting, and standing position. Measurements should be taken after 10 minutes of resting/laying, and immediately, after 2, 5, and 10 minutes of standing (if the patient is able).
Treatment can include a variety of drug related options, as well as lifestyle changes that help improve symptoms in some. Again, this will vary greatly from patient to patient, as the underlying cause of POTS impacts how a patient will respond.
Common lifestyle adjustments include increasing fluid and sodium intake to help retain fluids and expand blood volume, wearing compression stockings to prevent blood pooling, and exercising regularly. De-conditioning greatly affects POTS in most cases, and keeping as active as possible is extremely important.

Quality of Life & Outlook:
 POTS patients’ quality of
life can vary greatly, due to many things that cause POTS. It is not
contagious, is not life threatening, and generally improves with time
and treatment adjustments. It can be extremely disabling though, and
frustrating for patients and caregivers to cope with. Symptoms can
change from day to day, and hour to hour, and this makes it difficult
for physicians to treat as well.
POTS patients’ quality of
life can vary greatly, due to many things that cause POTS. It is not
contagious, is not life threatening, and generally improves with time
and treatment adjustments. It can be extremely disabling though, and
frustrating for patients and caregivers to cope with. Symptoms can
change from day to day, and hour to hour, and this makes it difficult
for physicians to treat as well. Treatment is usually focused on managing the symptoms and underlying causes, and there is no cure for POTS per say, since it is a syndrome (and not a disease). But if the underlying cause is treated, POTS symptoms may abate.
Many teens outgrow POTS or learn to live a highly functional life while managing symptoms. For others, POTS may go into remission, and flare up again, often with new and confusing symptoms. For an estimated 25% of the POTS population, quality of life is compared to those with Congestive Heart Failure or Chronic Obstructive Pulmonary Disease. This severely limits day to day activities such as work, school, and other lifestyle issues such as hygiene and childcare. There have been no long term studies with concrete numbers regarding the long term outlook for POTS patients.
The good news is that there is exciting research taking place, and many more resources for patients and families as they adjust to life with POTS. Find links to many of them on this website, including listings of support groups, tips and tools for patients, and treatment options.
Sources:
1. The Postural Tachycardia Syndrome (POTS): Pathophysiology, Diagnosis & Management. Raj SR, Indian Pacing Electrophysiology J. 2006 April-Jun; 6(2): 84-99.
2. Medical Dictionary, Medline Plus, U.S. Library of Medical Sciences and National Institutes of Health
3. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Freeman R et al. , Auton Neurosci. 2011 Apr 26;161(1-2):46-8. Epub 2011 Mar 9.
4. Postural Tachycardia Syndrome. Grubb BP, Circulation. 2008; 117: 2814-2817.
5. Postural tachycardia syndrome (POTS). Low PA, Opfer-Gehrking TL, Textor SC et al.
Neurology 1995; 45: S19-S25.
6. Sleep Disturbances and Diminished Quality of Life in Postural Tachycardia Syndrome. Raj SR.. J Clin Sleep Med. 2011 April 15; 7(2): 204–210.
7. The Autonomic Dysfunction Consortium, National Institutes of Health Rare Diseases Network
8. A review of postural orthostatic tachycardia syndrome. Carew et al., Europace (2009) 11 (1): 18-25.
9. Postural tachycardia in children and adolescents: what is abnormal? Singer W, Sletten DM, Opfer-Gehrking TL, Brands CK, Fischer PR, Low PA, J Pediatr. 2012 Feb;160(2):222-6. Epub 2011 Oct 11.
10. Vanderbilt Autonomic Dysfunction Center
Written by Claire Martin of Dysautonomia SOS, email with any questions at claire@dysautonomiaSOS.org.
Here are a few links to great summary articles about Orthostatic Intolerance and POTS.

No comments:
Post a Comment